Central Retinal Vein Occlusion

Central retinal vein occlusion (CRVO) occurs when the main retinal vein is blocked. This occurs at the narrow exit point through the optic nerve near the lamina cribrosa. Arteriosclerotic changes in the artery compress the vein leading to clot formation within the vein. Because blood can no longer travel smoothly out of the retina, it fills with blood and becomes swollen.
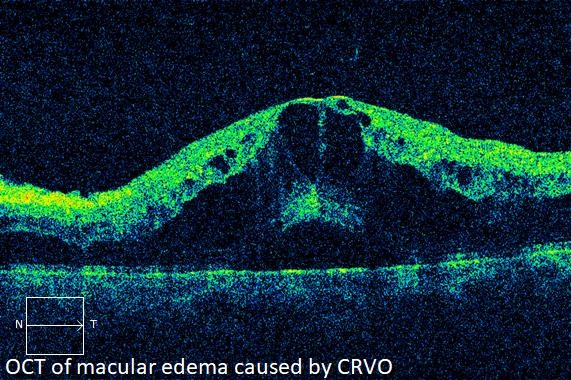
In response to the blockage, the body releases a protein called vascular endothelial growth factor (VEGF). This protein causes increased vascular permeability and induces neovascularization, the growth of abnormal blood vessels. Increased vascular permeability leads to leakage of fluid from vessels, and will often cause retinal swelling. Swelling in the central retina is called macular edema, which can result in loss of vision.
Further visual loss may develop if abnormal blood vessels break and bleed into the vitreous cavity, causing a vitreous hemorrhage. If neovascularization develops on the iris, blockage of the eye’s drainage system often occurs. This leads to marked elevation of eye pressure with secondary loss of vision and eye pain; a condition called neovascular glaucoma.
CRVO is most common in people with high blood pressure, diabetes, hyperlipidemia, or glaucoma. It is also more prevalent in those who smoke or use oral contraceptives.
SYMPTOMS
If the blockage is partial, the retina may continue to function adequately. Patients with CRVO usually experience blurred vision from retinal hemorrhage and macular edema. Spots, strands, or curtains in the vision may occur due to vitreous hemorrhage. Eye pain is usually due to neovascular glaucoma.
EVALUATION
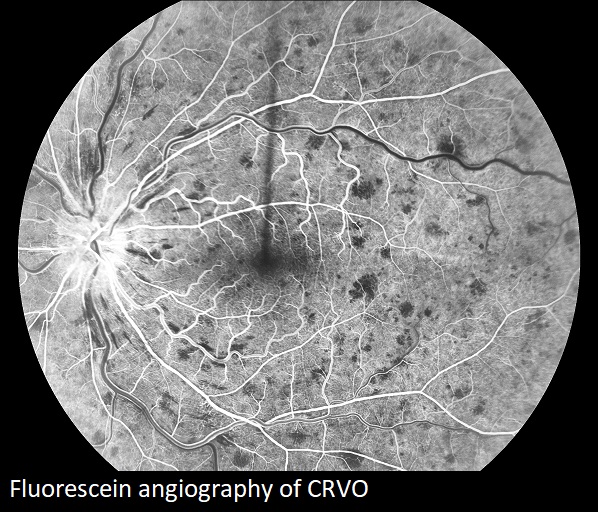
In addition to a dilated eye exam, fluorescein angiography may be performed during which dye is injected into a vein in the arm. Digital images of the retina are obtained as the dye passes through the eye. Blocked blood vessels, edema, and areas of ischemia and neovascularization then become detectable to the physician.
Optical coherence tomography (OCT), a scanning laser which images a slice or cross section of the retina, may be performed to determine if macular edema is present.
Ultrasonography may be used to determine the status of the retina when the view is obscured by vitreous hemorrhage.
Intravitreal injection
These tests aid in diagnosis and help establish the type of treatment needed. They are also useful in monitoring disease progression and response to therapy.
TREATMENT
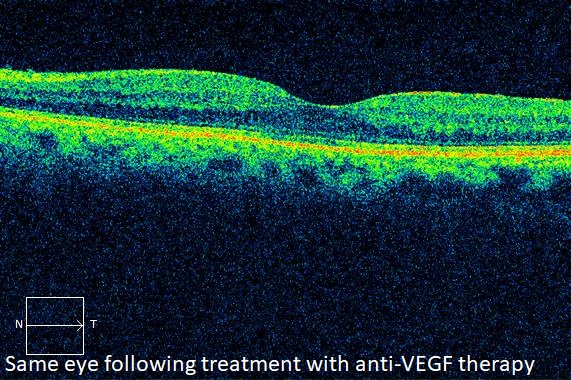
Intravitreal drug therapy improves the outcome in patients with CRVO. This procedure involves placing medication into the vitreous cavity of the eye. The injected medication acts upon damaged blood vessels to reduce leakage and resolve macular edema.
Anti-VEGF medicine is the first line treatment. Steroid implants or injections are considered in recalcitrant cases. Intravitreal drug therapy may also be recommended to cause regression of neovascularization. The therapy may involve ongoing treatments, sometimes over many years.
Laser treatment called panretinal photocoagulation (PRP) is often required when CRVO causes complications such as neovascularization of the iris or retina. Laser treatment is used to reverse growth of the new blood vessels, and can be used in combination with intravitreal drug therapy. Laser may be applied in several sessions.
Vitrectomy may be indicated in patients who develop vitreous hemorrhage. During this surgical procedure, the vitreous gel and blood are removed, and microscopic forceps are used to remove scar tissue. Leaking blood vessels are then cauterized and laser is applied. This is an outpatient procedure performed at the surgery center under local anesthesia.
Prognosis
Mild cases of CRVO often follow a benign course with about half maintaining good vision. In more severe or worsening cases, the visual prognosis without treatment is poor.
Eyes treated with anti-VEGF medicines such as Avastin, Lucentis, or Eylea, have a much more favorable prognosis, with the majority gaining significant vision. Treatment with these medicines is especially effective when macular edema is present.
Steroid treated eyes also demonstrate significant gains in vision but carry a higher risk for complications such as steroid induced cataract and glaucoma.
COMPLICATIONS
Complications from CRVO include those induced by the disease such as macular edema, retinal ischemia, vitreous hemorrhage, and neovascular glaucoma.
Treatment for CRVO also carries risks. Intravitreal injections may lead to infection, called endophthalmitis. Furthermore, retinal detachment or vitreous hemorrhage may occur following injection therapy.
Laser treatment risks include bleeding, and a reduction in peripheral and night vision.
Risks associated with vitrectomy include retinal detachment, vitreous hemorrhage, cataract, and infection.
When complications occur, prompt assessment and intervention may limit the damage to the eye.
From the Expert…
CRVO is a frequently encountered retinal disease. Risk factors include age, glaucoma, or vascular diseases including hypertension, hyperlipidemia, and diabetes. Furthermore, smoking and taking oral contraceptives increase the risk in otherwise healthy individuals. When no underlying risk factor is present, a workup searching for a hypercoagulable disorder may be performed.
Until recently, CRVO was untreatable except in severe cases with neovascular complications. Laser photocoagulation was used to prevent loss of the eye, but was not effective in restoring vision.
Currently, pharmacologic therapy with intravitreal anti-VEGF injections are very effective in reversing the damage of CRVO and restoring vision. Steroid injections and implants are also effective, but are usually considered as second line therapy due to their increased risk profile including cataract and glaucoma. These treatments wear off in several weeks to a few months, and usually must be repeated at regular intervals, sometimes for years.
Complications of treatment are uncommon and include infection, hemorrhage, or retinal detachment.
With accurate diagnosis, thorough assessment, and effective treatment, the majority of patients with CRVO can experience improvement in their condition and, importantly, their vision.
ADDITIONAL RESOURCES
American Academy of Ophthalmology Retina/Vitreous Panel. Preferred Practice Pattern® Guidelines. Retinal Vein Occlusions. San Francisco, CA: American Academy of Ophthalmology; 2015. Available at: www.aao.org/ppp.
Pichi F. Central Retinal Vein Occlusion. American Academy of Ophthalmology. EyeWiki. https://eyewiki.aao.org/Central_Retinal_Vein_Occlusion. Accessed July 24, 2019.
Retina Health Series. Central Retinal Vein Occlusion. The Foundation of the American Society of Retina Specialists. https://www.asrs.org/content/documents/fact_sheet_21_central_retinal_vein_occlusion_new.pdf. Accessed July 24, 2019.
Summary Benchmarks for Preferred Practice Pattern® Guidelines. Retinal Vein Occlusions. American Academy of Ophthalmology; 2018.
Yeh et al. Therapies for Macular Edema Associated with Central Retinal Vein Occlusion: A Report by the American Academy of Ophthalmology. Ophthalmology 2015;122:769-778.
