Why can't my patient see following cataract surgery?
Following cataract extraction, the majority of patients experience improvement of vision. Occasionally, vision improvement is less than expected, sometimes markedly so. This is a review of the common causes of poor visual results following cataract surgery.
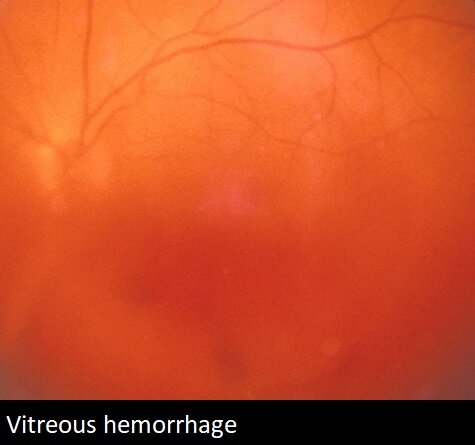
Surgical complications such as infection, vitreous hemorrhage, or retinal detachment are well known causes of post cataract extraction vision loss. Cystoid macular edema is a more common post surgical condition which is usually responsive to treatment. Corneal edema is also a possible complication of cataract extraction.
A common reason for unsatisfactory improvement in vision after cataract extraction is the presence of preexisting disease:
Amblyopia
Amblyopia or lazy eye is a condition in which the visual system of one eye does not develop in childhood. This can be masked during cataract progression, though limits recovery of vision following surgery.
Refractive error
Postoperatively, dependency on glasses is usually decreased. Sometimes an updated refraction will solve the patient’s visual difficulties.
Cornea
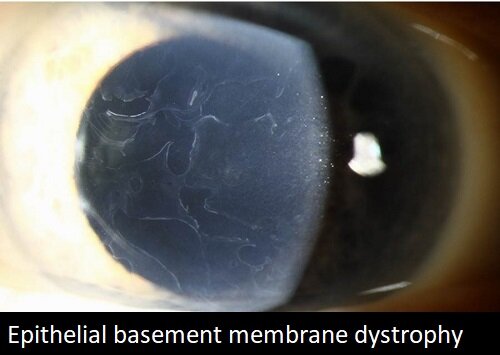
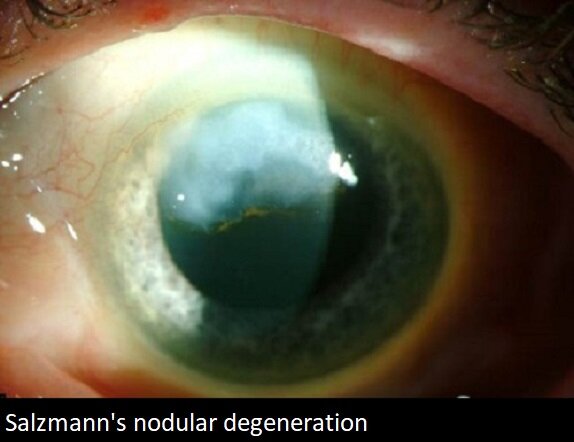
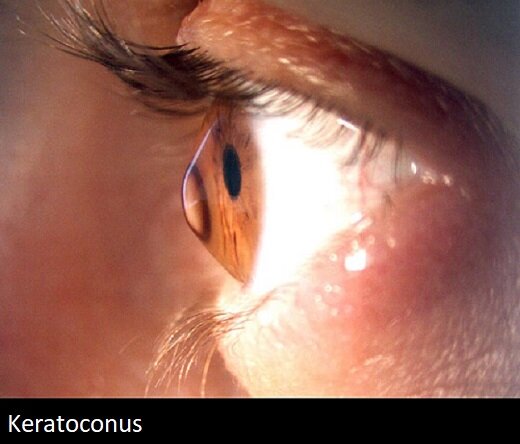
The cornea is a clear dome that covers the eye. Subtle corneal disease can alter a patient’s vision. Problems such as epithelial basement membrane dystrophy, Salzmann’s nodular degeneration, Fuchs’ corneal dystrophy and secondary post-surgical edema, and keratoconus, all alter the image transmitted through the cornea into the eye. Even when the findings are subtle, their impact can be substantial and limit vision recovery following cataract extraction.

Intraocular lens
With cataract surgery, a synthetic lens is placed into the capsular space. The capsule is supported by fibers called zonules. If the zonules are weak or damaged, the lens may slip out of its optimal position, affecting vision.
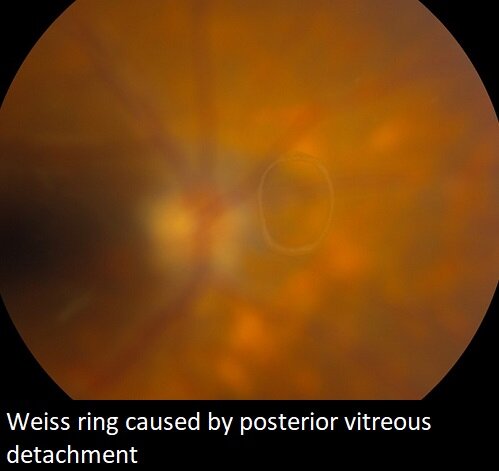
Vitreous
Vitreous is the clear gel that fills the eye. Vitreous opacities can alter a patient’s vision.

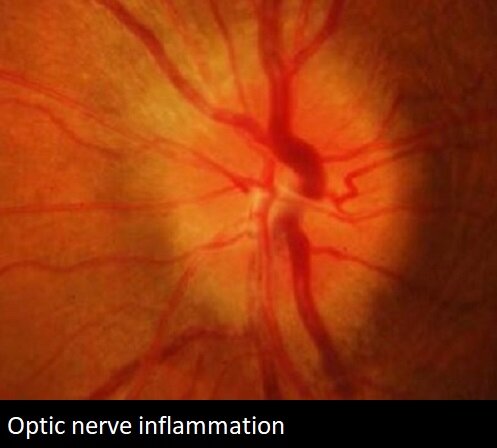
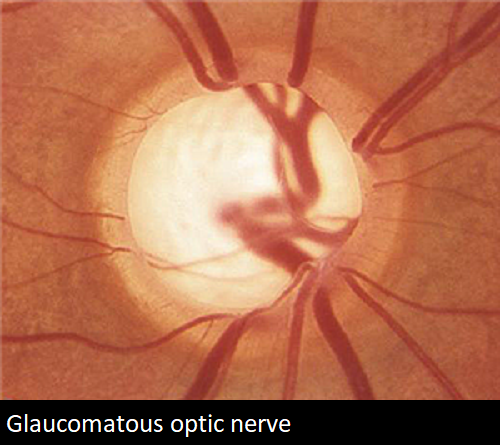
Optic nerve
The optic nerve is the nerve that transmits vision from the eye to the brain. Previous optic nerve disease such as ischemia, inflammation, infection, or glaucoma may diminish the visual recovery possible with cataract surgery.
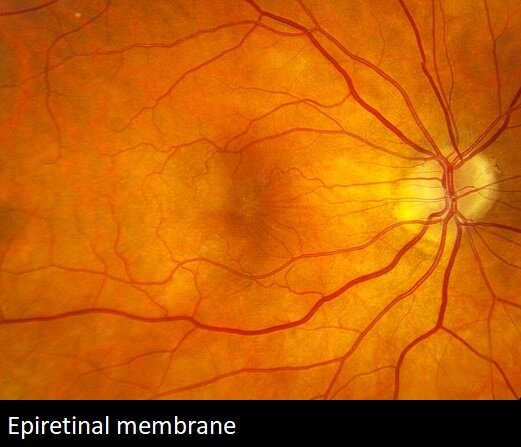
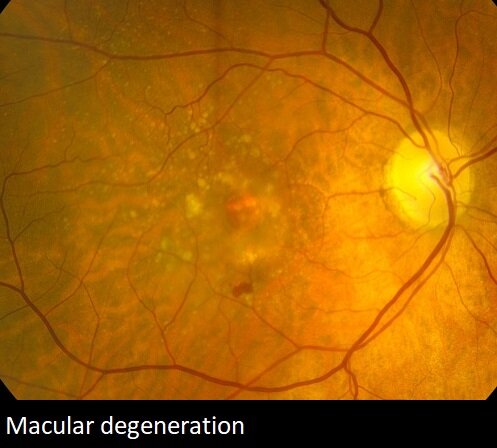
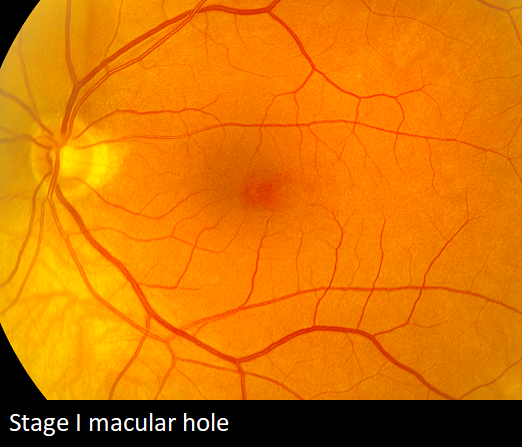
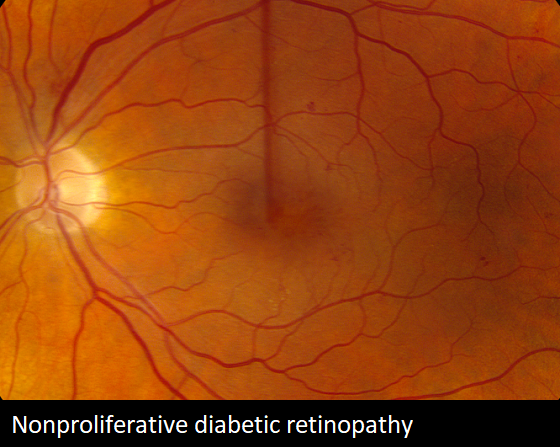
Macula
The macula is the center of the retina responsible for fine work such as reading and driving. Maculopathy, whether from macular degeneration, epiretinal membrane, macular edema, macular hole, or diabetic retinopathy will diminish the quality of the image captured by the retina and the patient’s vision after cataract removal.
Intracranial/occipital
The visual pathway travels through the brain and ends in the occipital cortex where the image is visualized. Any injury to this visual system, including aneurysm, tumor, or stroke, will limit visual recovery following cataract surgery.
From the Expert…
Cataract extraction is the most commonly performed ocular surgical procedure in America. The vast majority of patients experience significant improvement in their vision.
Occasionally, surgical complications such as capsular rupture, vitreous loss, or retained lens material can lead to conditions which will limit the patient’s visual recovery. These include cystoid macular edema, infection or retinal detachment. When these conditions occur, a vitreoretinal surgeon is usually necessary to address them. With effective intervention, the majority of patients experience improvement in their ocular health and some restoration of vision.
Preexisting conditions are also a common cause for suboptimal recovery of vision following cataract extraction. They are often times unknown or underappreciated prior to surgery. They become apparent after the cataract has been removed, and the vision does not recover as anticipated. Often times, these are long standing problems and resistant to treatment. A thorough evaluation preoperatively can often times detect these conditions, and inform the patient and surgeon about the visual potential with cataract extraction.
