Post Injection Endophthalmitis
Endophthalmitis is a condition in which inflammation develops in the interior of the eye. Post injection endophthalmitis (PIE) refers to inflammation following intravitreal injection of medicine. Anti-VEGF agents are the most commonly injected medicines, though steroids, antibiotics, antifungals, and antivirals may also be injected. The majority of PIE cases are bacterial infections, but some are sterile, noninfectious inflammation.
Symptoms & Evaluation
PIE usually presents with redness, pain, light sensitivity, and decrease in vision.
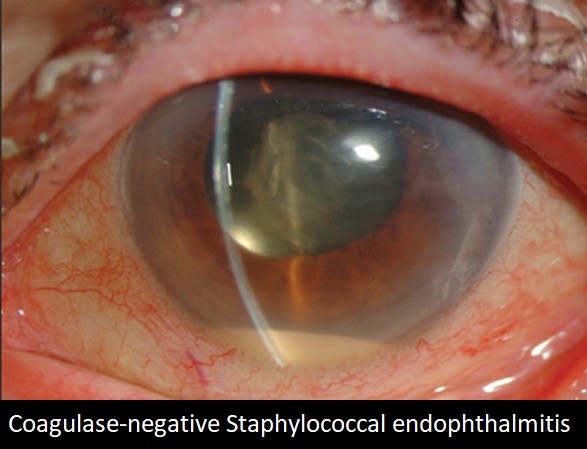
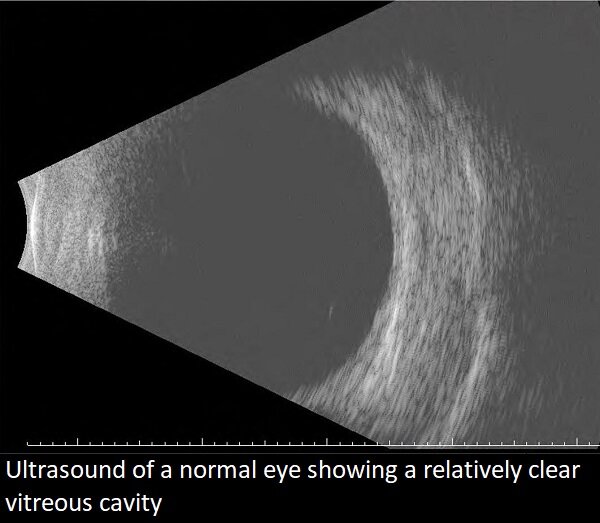
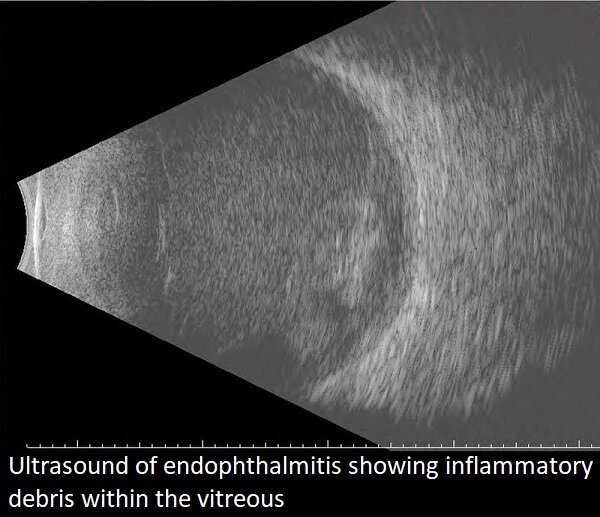
Findings include injection, or redness, of the conjunctiva, corneal edema, aqueous cells, hypopyon, fibrin membranes, and vitritis.
The diagnosis of PIE is made based on its characteristic clinical appearance and recent history of intravitreal injection.
Treatment

Once the diagnosis of PIE is established, treatment is recommended. Unless sterile inflammation is probable, antibiotics (vancomycin and ceftazidime) are given intravitreally. First, a vitreous and sometimes aqueous tap are performed to culture for organisms and decrease the internal volume of the eye, making room for the antibiotic medicine injected. Some surgeons also inject dexamethasone, a steroid, to decrease inflammation. I do not.
Some PIE patients will undergo pars plana vitrectomy (PPV). This surgical procedure debulks the vitreous cavity and allows a large sample for culture.
Pathogen
The majority of PIE cases are caused by bacterial infection. Coagulase-negative Staphylococcus is the most frequently isolated organism. Streptococcus, Staphylococcus aureus, and gram negative bacteria are less common.
Prognosis
The majority of patients with PIE experience an improvement in their clinical condition and vision after treatment. Coagulase-negative Staphylococcus and culture-negative cases experience the best outcome with vision of about 20/50 on average. Infection with Streptococcus portends a much worse prognosis.
Prevention
Of course, the best medicine for PIE is prevention. Prior to intravitreal injection, topical povidone-iodine, Betadine, is used to prep the conjunctiva, lashes, and lid margins. A lid speculum is recommended to ensure exposure to the injection site and keep lashes from contacting the needle. Careful technique is employed to keep the medicine and needle from being contaminated with bacteria. Prophylactic topical antibiotics are generally not used.
From the Expert…
Intravitreal injections are a very common procedure, performed approximately 6 million times a year in America. That number continues to grow as indications for anti-VEGF therapy increase and the population ages.
The incidence of PIE is low, currently approximately 0.02%, or 1/5000. This low rate is achieved by an effective prep and careful injection technique.
Treatment of PIE involves accurate diagnosis and urgent intervention with intravitreal antibiotics. The standard of care requires conscientious follow up to monitor for clinical response.
Some eyes suffer severe vision loss with PIE, even with effective management. Therefor, prevention is the best medicine.
Additional Resources
Xu et al. Endophthalmitis after Intrativreal Injection of Vascular Endothelial Growth Factor Inhibitors: Management and Visual Outcomes. Ophthalmology 2018;125:1279-1286.
Stem et al. Predictors of Endophthalmitis after Intravitreal Injection: A Multivariable Analysis Based on Injection Protocol and Povidone Iodine Strength. Ophthalmology Retina 2019;3 3-7.
Sachdeva et al. Endophthalmitis following intravitreal injection of anti-VEGF agents: long-term outcomes and the identification of unusual micro-organisms. Journal of Ophthalmic Inflammation and Infection 2016;6:2.
Gupta Y. Post Injection Endophthalmitis (PIE). EyeWiki. American Academy of Ophthalmology. https://eyewiki.aao.org/Post_Injection_Endophthalmitis_(PIE). Accessed October 9, 2019.
Retina Health Series. Endophthalmitis. The Foundation of the American Society of Retina Specialists. https://www.asrs.org/content/documents/fact_sheet_26_endophthalmitis_new.pdf. Accessed October 7, 2019.
