Anterior Uveitis
Uveitis
Uvea are the pigmented vascular layers of the eye within the iris, ciliary body, and choroid. Uveitis is inflammation of any of these structures.
Uveitis is typically described by its location, timing, and physical findings. Anterior uveitis refers to inflammation in the front of the eye. Posterior uveitis refers to inflammation in the back of the eye. Panuveitis refers to inflammation of the entire uveal tract. Uveitis can also be described as acute or chronic, and nongranulomatous or granulomatous.
Anterior Uveitis
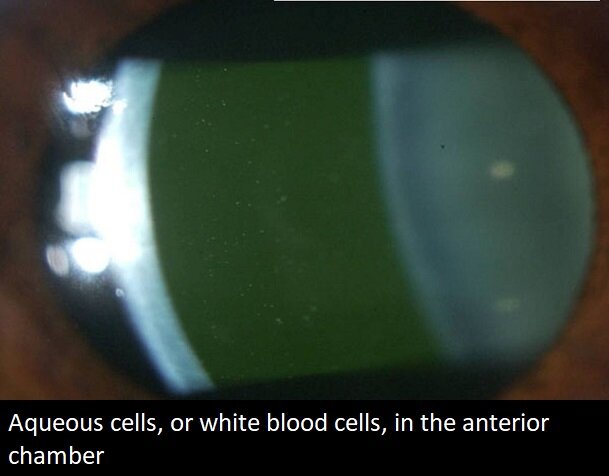
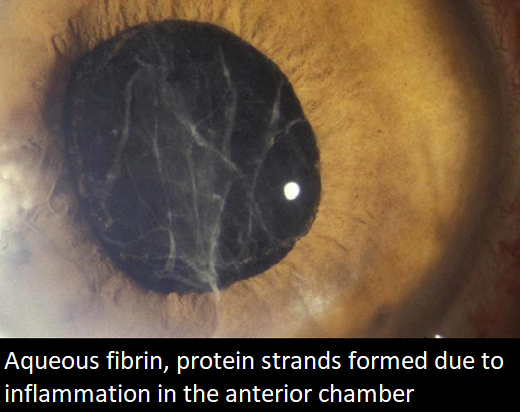
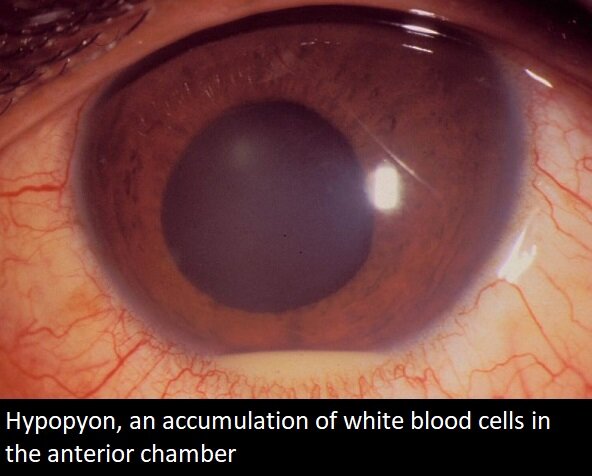
Anterior uveitis is inflammation of the anterior structures of the eye including the iris, ciliary body, and anterior chamber. Symptoms include redness, pain, photophobia, and decrease in vision. Findings on presentation include conjunctival injection, aqueous cells, corneal inflammatory deposits called keratic precipitates, and aqueous flare and fibrin. The incidence is about 1/10,000 per year.


In the majority of cases of anterior uveitis, there is no known cause. These are termed idiopathic. When a cause is present, the most common is HLA-B27 positivity. This represents a protein antigen which is on cell surfaces, which incites inflammation through many organ systems of the body. There are numerous systemic diseases including ankylosing spondylitis, Reiter’s syndrome, ulcerative colitis, Crohn’s disease, and psoriatic arthritis, which have uveitis as a component and HLA-B27 positivity.
Other causes of acute uveitis include juvenile rheumatoid arthritis, sarcoidosis, Fuchs’ heterochromic iridocyclitis, Behçet’s disease, glaucomatocyclitic crisis, and masquerade syndrome.
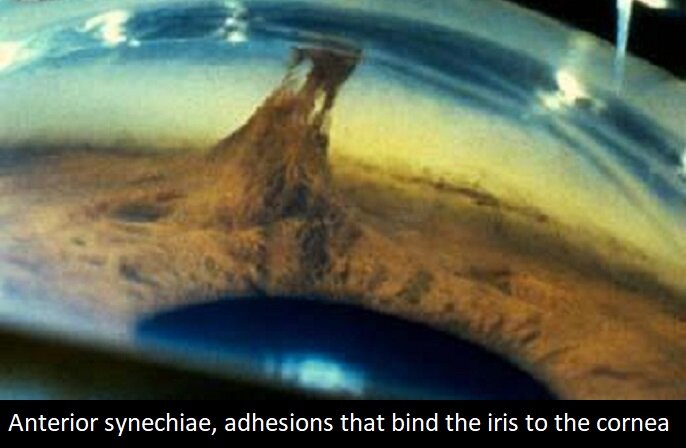
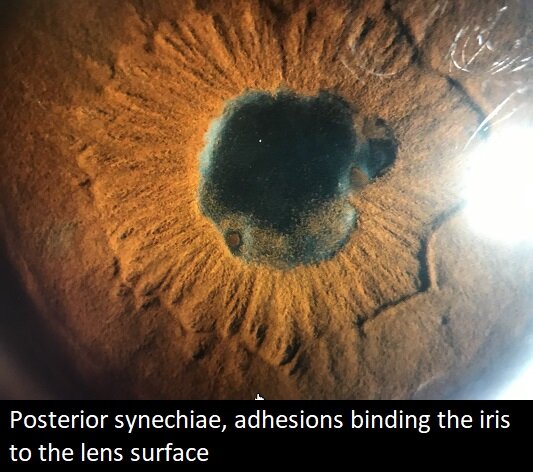
The goal of anterior uveitis treatment is to suppress the inflammation, improve the vision, and avoid scarring. Corticosteroids and cycloplegia are the mainstay of therapy. Steroids are administered orally, systemically, topically, periocularly, or intravitreally. Nonsteroidal antiinflammatory drugs (NSAIDs) are additive to steroids. They are especially useful in the setting of steroid induced glaucoma and may be safer for long term suppressive therapy. Cycloplegia, which leads to pupillary dilatation, is often administered to break synechiae and relieve pain.
In more severe and unresponsive cases of anterior uveitis, immunosuppressive therapy with methotrexate may be indicated. Biologic response modifiers such as Remicade (infliximab), Humira (adalimumab), and Enbrel (etanercept) are considered in chronic cases. When an infectious cause is suspected in anterior uveitis, such as toxoplasmosis, syphilis, Lyme, or herpes, antibiotics or antivirals may be given as well.
From the Expert…
Anterior uveitis is an inflammatory condition of the anterior structures of the eye. Numerous etiologies are known, most falling into the category of inflammation or infection. When an infection with either bacterial or virus is present, antibiotics or antivirals are necessary. Otherwise, steroids, NSAIDs, methotrexate, and biologic response modifiers make up the mainstay of treatment.
Work up is focused on the most common causes and include HLA-B27 and a CBC. Syphilis is often checked for, as it is the “great masquerader,” highly contagious, and treatable with appropriate antibiotics. A search for other conditions such as juvenile rheumatoid arthritis or sarcoidosis is pursued when there is suspicion for their presence.
Uveitis used to be a painful and blinding disorder. With ever advancing treatments, it is now controllable and often reversible. The majority of patients gain and keep their vision for the long term.
Additional Resources
Anterior Uveitis (Iritis/Iridocyclitis). The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease, Seventh Edition. Philadelphia: Lippincott, 2017.
LaMattina KC. Overview of Uveitis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/eye-disorders/uveitis-and-related-disorders/overview-of-uveitis#. Accessed 22 October 2019.
Harman LE, Margo CE, Roetzheim RG. Uveitis: The Collaborative Diagnostic Evaluation. Am Fam Physician 2014;90:711-716..
Guney E and Tugal-Tutkun I. Symptoms and Signs of Anterior Uveitis. US Ophthalmic Review 2013;6:33-37.
