Age-Related Macular Degeneration
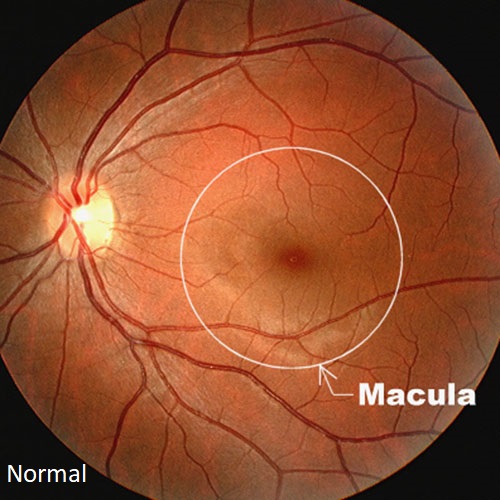
Age-related macular degeneration (AMD) is a disease that causes damage to the macula, located in the center of the retina. The macula is responsible for fine vision. When the macula does not function correctly, central vision may be blurred, distorted, or darkened. Macular degeneration is the leading cause of visual impairment in people 65 years or older, being more common in those with a fair complexion. While macular degeneration is most common in people over the age of 60, it may develop earlier. It often runs in families.
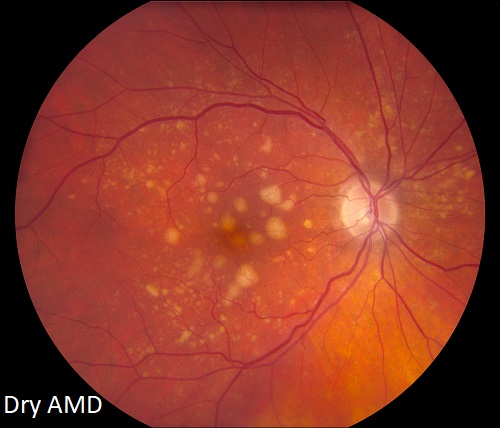
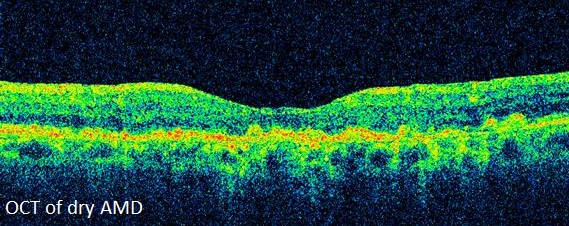
Dry Macular Degeneration (Dry AMD)
Dry, or non exudative, macular degeneration is the most common form of the disease, occurring in approximately 90% of patients with macular degeneration. Dry AMD results when protein deposits called drusen develop under the macula. Thinning, or atrophy, of the retina may also occur. Dry AMD is divided into four categories: early, intermediate, advanced without subfoveal involvement, and advanced with subfoveal involvement.
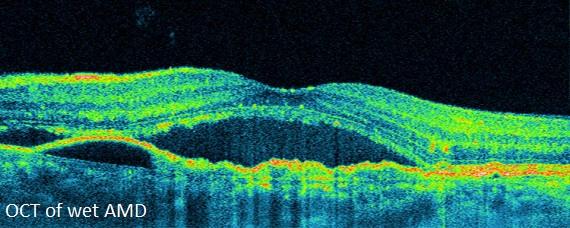
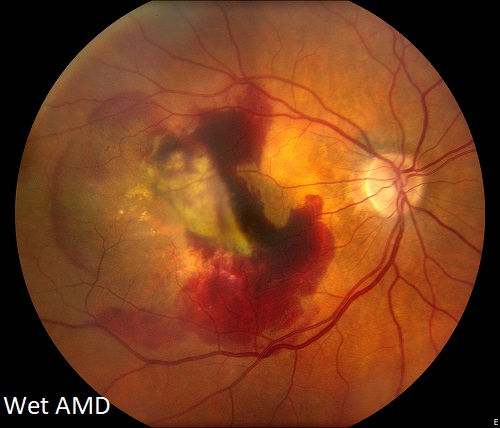
Wet Macular Degeneration (Wet AMD)
In some patients, dry macular degeneration will progress to wet, or exudative, macular degeneration, in which abnormal blood vessels grow under the retina occurring in areas weakened by drusen or atrophy. This is called a choroidal neovascular membrane (CNVM) or subretinal neovascular membrane (SRNVM). These new blood vessels then leak serum and lipid, and may also bleed. Scar tissue forms over time, causing a permanent dark spot in the center of vision.
Symptoms
Macular degeneration can cause various symptoms, while in its earliest stages may even be asymptomatic. If the disease progresses, blurred or distorted vision is common. A central dark or blind spot can also occur. It is possible for vision to deteriorate in one eye while the other one continues to see well for many years. When both eyes are affected, loss of central vision may be noticed immediately. Dry AMD tends to progress slowly, with vision often remaining normal. When vision loss does occur, it usually advances slowly due to thinning or atrophy of the macula. In Wet AMD, there is often sudden loss of vision. Macular degeneration can make some activities such as driving or reading difficult, if not impossible. Although the condition might reduce central vision, it does not affect peripheral vision.
Evaluation
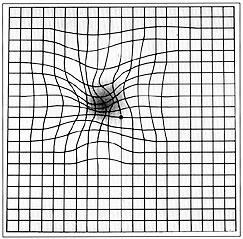
A thorough eye examination will determine if macular degeneration is present. A simple vision test using a grid resembling graph paper (an Amsler grid) is helpful in detecting vision abnormalities due to retinal disease.
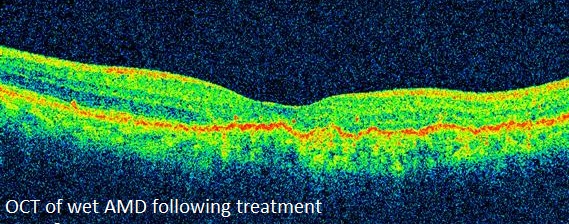
Optical coherence tomography (OCT) is a scanning laser used to image a slice of the retina in cross section. OCT is useful in detecting fluid in the macula and for monitoring improvement following treatment.
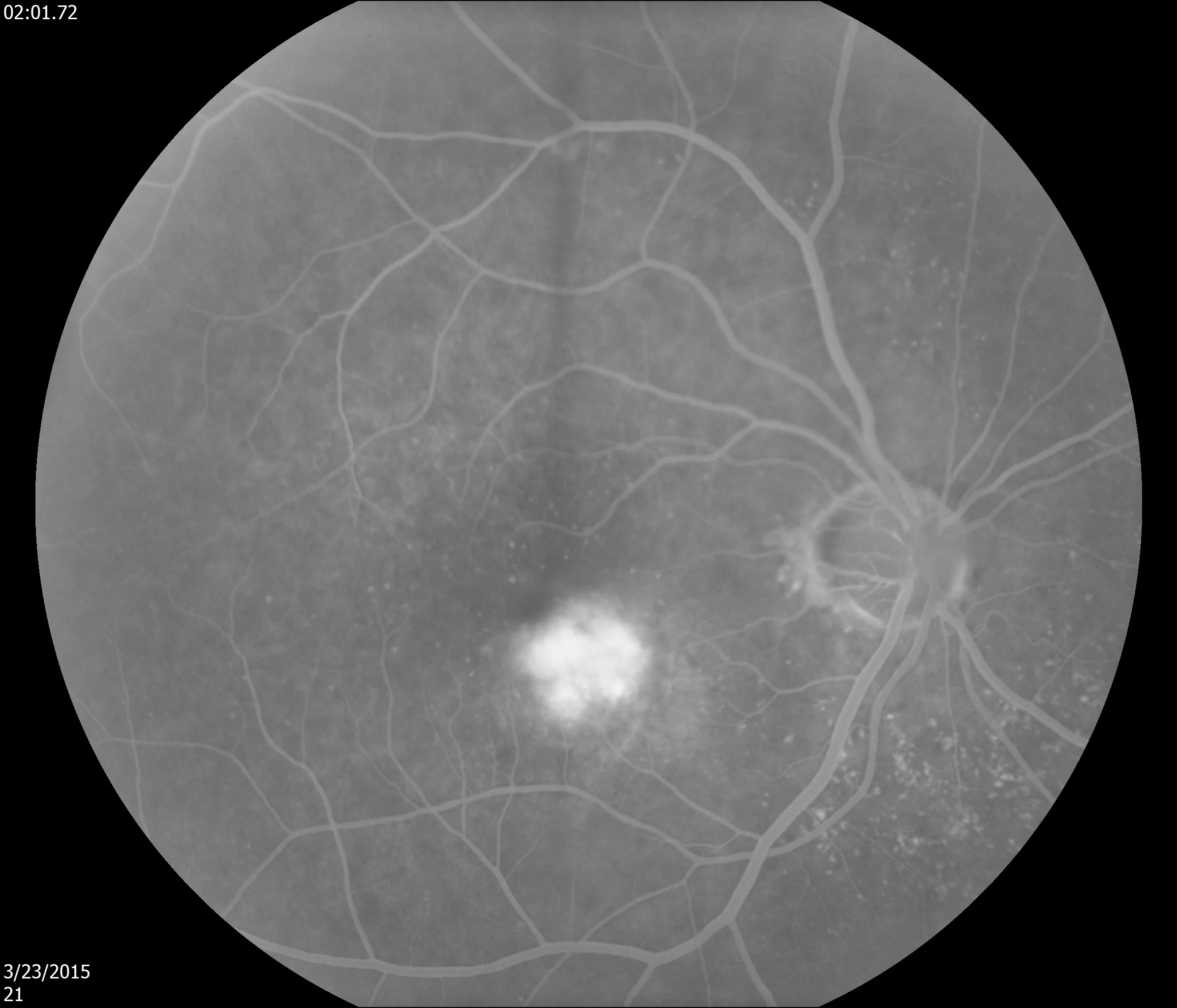
A test called fluorescein angiography may be required during which dye is injected into a vein in the arm. Digital images of the retina are obtained as the dye passes through the eye. The abnormal blood vessels leak the injected dye, becoming detectable to the physician.
Indocyanine green angiography (ICG) is an imaging test which concentrates on the choroidal blood vessels which are the source of the neovascularization. This test is especially useful in atypical cases.
Amsler grid showing a simulation of distorted vision caused by AMD
Fluorescein angiography of wet AMD. Abnormal vessels appear white.
Treatment
Macular Degeneration & Nutrition
The Age-Related Eye Disease Study (AREDS) demonstrated that therapeutic dosages of antioxidants and zinc decrease the progression of macular degeneration.
The Age-Related Eye Disease Study 2 (AREDS 2) was designed to learn more about the role of vitamins and minerals in preventing vision loss from AMD. This study ran for five years, monitoring 4,000 patients. Results confirmed the benefits of vitamins and minerals in helping to prevent vision loss from AMD. It is recommended that individuals taking supplements for macular degeneration use the “AREDS 2 formula.”
AREDS 2 recommended daily dosages: Vitamin C 500 mg, Vitamin E 400 IU, Lutein 10 mg, Zeaxanthin 2 mg, Zinc 80 mg, Copper 2 mg
AREDS 2 supplements have proven to lower the risk of disease progression by 25% in patients with at least intermediate dry AMD. The study showed no benefit to those with early or no AMD.
Eating dark green vegetables and fish may lower the rate of vision loss for patients with AMD. Smoking substantially increases the risk of vision loss, and patients should be counseled on smoking cessation.
Intravitreal Drug Therapy
Intravitreal drug therapy
Intravitreal drug therapy is the preferred technique for treating Wet AMD. A number of medicines have been developed which inhibit growth of the abnormal vessels beneath the retina in Wet AMD. These include Avastin (bevacizumab), Lucentis (ranibizumab), and Eylea (aflibercept). The medication is placed directly into the eye with a fine needle. The procedure, usually performed in the office, is well tolerated. Most eyes receiving intravitreal injections for new onset Wet AMD will have stable or improved vision. To maintain vision, these injections often are repeated at four to twelve-week intervals, sometimes for the life of the patient.
Laser Treatment
Laser treatment used to treat Wet AMD is a brief and painless in-office procedure during which a highly focused beam of light is used to destroy the leaking blood vessels that damage the macula. Although a small, permanent “blind spot” is left at the point of laser contact, the procedure can preserve more overall sight. This treatment is usually recommended when abnormal blood vessels have not yet grown under the center of the macula. Pretreatment with intravitreal drug therapy may help to make laser treatment more successful.
Complications
Intravitreal injections carry with them certain risks. These include infection, sterile inflammation, hemorrhage, or retinal detachment. While, uncommon, these complications can lead to severe vision loss, even when managed correctly.
Because complications may occur, patients are usually evaluated if their eye becomes painful, light sensitive, or if the vision is substantially altered. If a complication is detected, antibiotic injection and/or surgery may be necessary to preserve or restore vision.
From the Expert…
Macular degeneration is a common disease in America’s aging population. While dry AMD is more common, wet AMD is associated with greater risk for vision loss.
The standard of care in managing dry AMD includes high dose vitamins, smoking cessation, and evaluations as indicated. Patients should be educated on methods to assess their own visual acuity and detect new symptoms.
The standard of care for wet AMD usually involves intravitreal drug injections. With this treatment, the majority of patients experience stability or improvement in vision. A delay in treatment can result in severe, permanent vision loss.
Complications, while uncommon, may be severe. They include infection, bleeding, and retinal detachment. The outcome following a complication is variable, but usually improved if the condition is diagnosed early and appropriate treatment is provided.
Additional Resources
American Academy of Ophthalmology Retina/Vitreous Panel. Preferred Practice Pattern®Guidelines. Age-Related Macular Degeneration. San Francisco, CA: American Academy of Ophthalmology; 2015. Available at: www.aao.org/ppp.
Elshatory Y. Age-related macular degeneration. American Academy of Ophthalmology. EyeWiki. https://eyewiki.aao.org/Age-related_macular_degeneration. Accessed July 9, 2019.
Retina Health Series. Age-Related Macular Degeneration. The Foundation of the American Society of Retina Specialists. https://www.asrs.org/content/documents/fact_sheet_16_amd_new.pdf. Accessed July 9, 2019.
Summary Benchmarks for Preferred Practice Pattern® Guidelines. Age-Related Macular Degeneration. American Academy of Ophthalmology; 2018.